News
Lawmakers Try Final Push On Bill To Regulate “Step Therapy” By Insurers
By: Karen Kasler | Statehouse News Bureau
Posted on:
A bipartisan bill dealing with how insurance companies deny certain treatments and drugs until other options are tried first is getting a final push in this lame duck session. And there’s a lawmaker who’s joining in on this effort – but as a patient.
It’s called “step therapy” – where insurers deny a drug or treatment until a different, sometimes cheaper option is tried first.
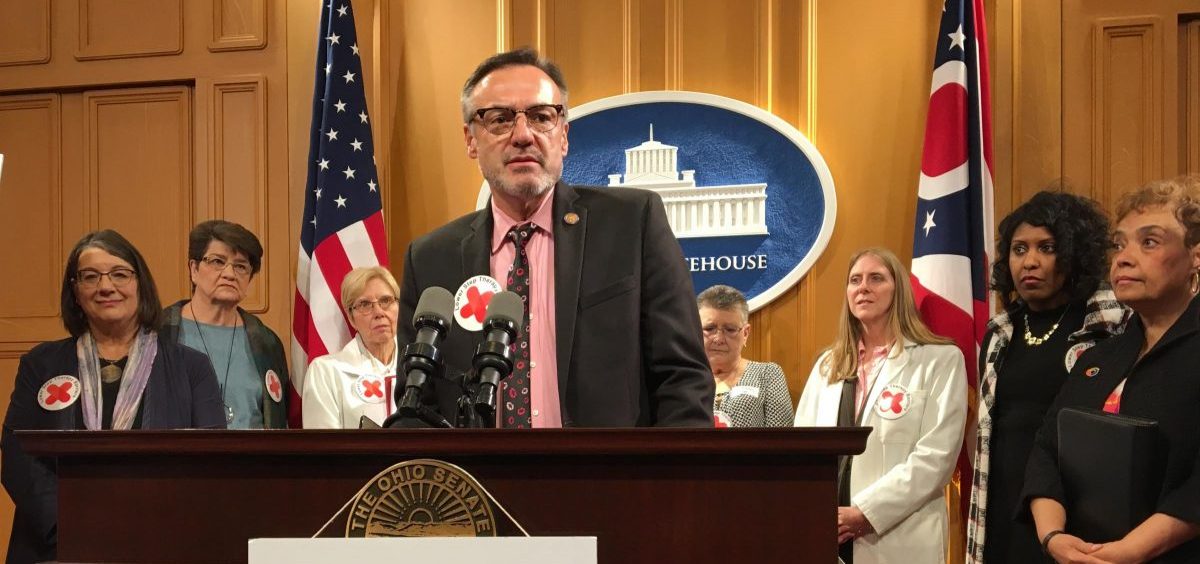
Rep. Scott Lipps (R-Franklin) came face to face with it after fell seriously ill and was denied the drug his specialist had prescribed in favor of a medication he says did nothing but cost him recovery time. “I learned this new term ‘step therapy’ in a very negative personal matter. And when I learned I had colleagues working on this issue, I was standing behind them cheering them on,” Lipps said.
Lawmakers say they want to ensure there’s a clinical reason for step therapy, and that it’s not just to save money. Health plans have opposed this bill, saying step therapy ensures safer, more cost-effective drugs are used first.

