News

Ohio Valley Facing Pandemic With a Health System Hollowed Out by Hospital Closures
< < Back to ohio-valley-facing-pandemic-with-a-health-system-hollowed-out-by-hospital-closuresAs new cases of coronavirus mount in the Ohio Valley, health officials are bracing for an onslaught of patients and what could be unprecedented demand for beds, medical staff and specialized equipment.
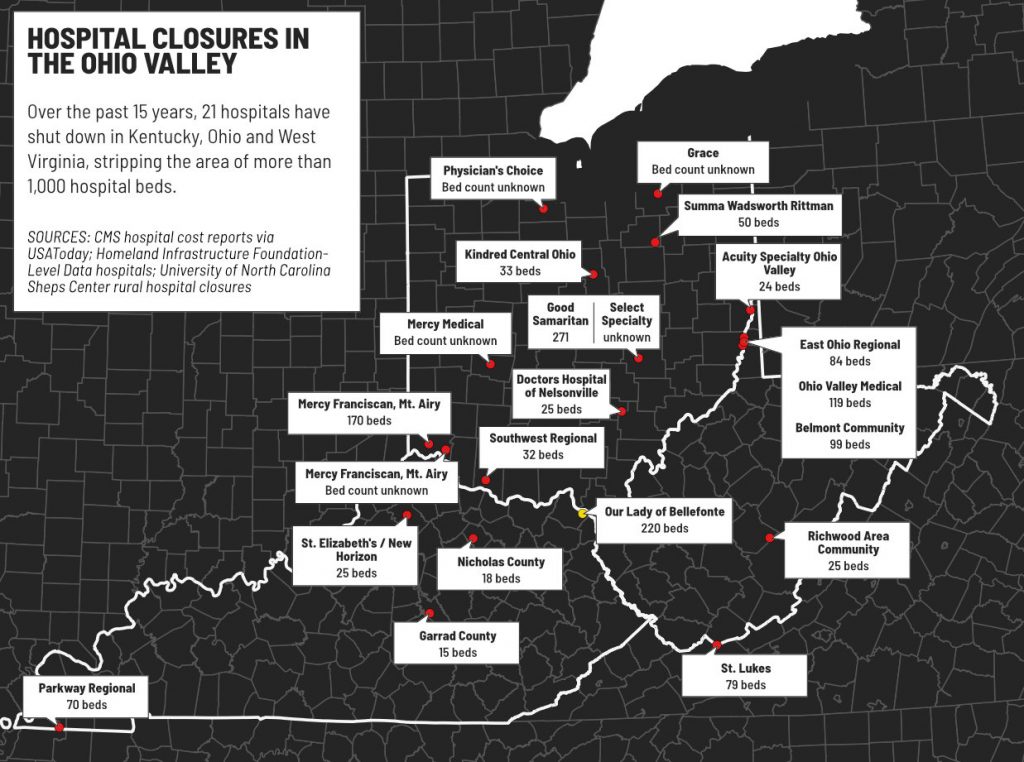
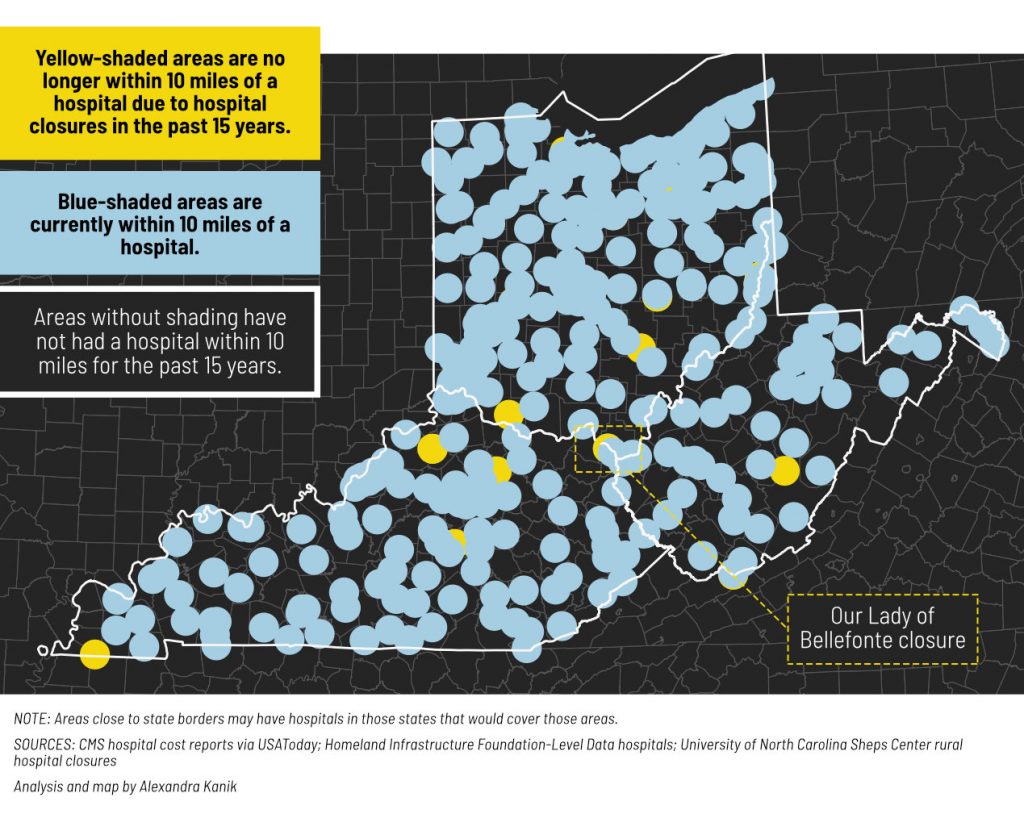
Kentucky, Ohio and West Virginia have disproportionately high rates of people vulnerable to serious illness from COVID-19. But the region’s capacity to treat them has been sharply reduced by the closure of some 21 hospitals over the past 15 years. An analysis by the Ohio Valley ReSource shows some of the communities where hospitals have closed have some of the nation’s poorest health outcomes, making them especially vulnerable.
Still more hospitals in the region are being closed now, even as the pandemic unfolds.
Tiffany Wilburn-Meeks has lived in eastern Kentucky’s Greenup County for most of her 38 years. And the hospital her family has always relied on is only a five-minute drive away.

“But I think if she’d had to go to King’s Daughters [Hospital], I don’t know that she would have survived the drive because it’s 10 or 15 more minutes down the road.”
But by May, her family won’t be able to rely on Our Lady of Bellefonte anymore. The 220-bed hospital with more than 1,000 employees — started by a congregation of Catholic sisters in 1953 with the blessing of the pope via telegram — will close its doors.
That would leave 35,000 people in Greenup County without a hospital, forcing those who need intensive medical care to drive to King’s Daughters Hospital in Ashland. This comes as many Ohio Valley public health officials are bracing for the coronavirus to reach their communities.
While the number of confirmed cases in her region have not reached levels in larger cities, she knows the number will grow.
“If it does, there’s no way that King’s Daughters is going to be able to handle that,” she said. “It is terrifying, and I’m afraid that people will die as a consequence of the hospital closing.”
In a statement, a spokesperson for King’s Daughters Hospital said they were working daily with Our Lady of Bellefonte to potentially expand the capacity of King’s Daughters if patient needs surge due to coronavirus.

These closures have left a hollowed out healthcare infrastructure in the Ohio Valley, and leading healthcare professionals worry that the loss of hospital beds, skilled staff and equipment — combined with a population that is especially vulnerable to COVID-19 disease — could hinder how well the region can respond to the coronavirus.
Running Out
For 15 years, Marlene Moore was lead nurse of the intensive care unit at Ohio Valley Medical Center in downtown Wheeling, West Virginia. She would make determinations about who would be admitted and who would be discharged, who would be transferred to other departments and hospitals, and helping younger nurses with questions and assistance.
That time came to an end when the company that owned OVMC and another hospital in nearby Martin’s Ferry, Ohio, announced last year both hospitals would close. Along with Belmont Community Hospital also closing, three hospitals in total last year shuttered in the Wheeling metropolitan area.

Moore started working last month at what is now the only hospital in town, Wheeling Hospital, where a coronavirus patient is currently being treated.
She said because Wheeling Hospital often has many beds filled with patients having other needs, those needing a bed for coronavirus treatment may have to travel a half-hour or more to hospitals in Steubenville, Ohio, Columbus or Pittsburgh.
And it’s the kind of people her hospital tends to serve that has her particularly worried.
“We have such an older population here. And if you get several that come in at the same time with severe respiratory distress, you’re going to run out of ICU beds, you’re going to run out of ventilators, you’re actually going to run out of places to treat these people,” she said.
A recent Kaiser Family Foundation study found West Virginia led the nation in how vulnerable its population is to coronavirus because of old age and preexisting conditions. More than half of all adults in West Virginia and more than 45% of all adults in Kentucky were at high risk of serious illness from coronavirus because of advanced age, pre-existing conditions, or both.
A report from Kaiser Health News also found there are only 325 ICU beds for more than 12,000 people over the age of 60 in Ohio County, where Wheeling is located. People over the age of 60 make up 28% of the county’s population.
According to an Ohio Valley Resource data analysis, 4 of the 18 counties that lost hospitals over the past 15 years also have some of the worst health outcomes in the nation. Those counties have some of the country’s highest rates of chronic respiratory disease deaths, cardiovascular disease deaths and diabetes prevalence.
Amid closures, remaining Ohio Valley hospitals are reinforcing their capacity for beds, equipment and personal protective equipment for worst case scenarios.
A statement from the West Virginia Hospital Association said hospitals are canceling or rescheduling elective surgeries to free up more beds, in compliance with a state emergency order. Hospitals are converting different departments into infectious disease units, and developing “alternative treatment sites.” One hospital in Athens, Ohio, has now set up a triage tent to treat potential patients outside.
Rising Costs
Even if Ohio Valley hospitals are able to accommodate a surge of coronavirus patients, the financial toll it could take could devastate rural healthcare providers.
A report last year from Navigant Consulting showed that 16 rural hospitals in Kentucky — about a quarter of all rural hospitals in the state — were at high risk of closing due to unstable financial situations. Some of the reasons cited for financial struggles include population loss with fewer people to serve, and more patients insured through Medicare and Medicaid, which often undercompensates hospitals for treatment.
Those ongoing challenges will only be made worse by the pandemic.
“The payment mechanism for treating these patients is not clear at this point. The unusually long length of stay I think is a concern with the very sick of these patients who typically end up, or have ended up, on ventilator care, which is very expensive and resource intensive to deliver,” said Bud Warman, Kentucky Hospital Association Vice President and former CEO of Highlands Regional Medical Center in east Kentucky. “They haven’t always had potentially this much volume of wants to deal with.”
The American Hospital Association is asking for $100 billion from Congress to offset anticipated coronavirus costs, while some rural hospitals struggle to ration protective medical supplies. A bill being considered by the Kentucky Senate would also provide a loan program for struggling rural hospitals.
Warman also said when hospitals have closed in Appalachia, there are often few options remaining for the people the provider served.
“In some cases, they just don’t have adequate transportation to get them that longer distance,” Warman said. “If they’re deciding between food on the table or traveling 50 miles to see a doctor or to seek health care, oftentimes, they make the choice for food on the table. It sounds dire, but the fact is in many parts of our state, many parts of Appalachia, that is the case.”
What’s Left
In central West Virginia, Michael Brumage is leading one of the remaining options for those without easy access to a hospital.
His staff is preparing to treat patients who have respiratory symptoms outside of the centers in order to prevent the spread of the virus inside their buildings, and they’ll also have curbside service for those with respiratory symptoms.

But even with his centers, there are still intensive, in-patient services that he can’t provide, that a hollowed out healthcare infrastructure has left lacking.
Brumage was born in Fairmont Regional Medical Center in Fairmont, West Virginia. So was his sister. He’s had several relatives who’ve been hospitalized there over the years. The hospital is set to close this week.
“It’s befuddling to me how they can close this hospital during a pandemic, when there are going to be so many more beds that need to be filled. It staggers the imagination,” Brumage said.
While a hospital is being built to replace Fairmont Regional, Brumage is worried that it will be too late for the demand for hospital beds, ventilators and skilled staff needed to respond to the pandemic.
“There will be many competing economic priorities once this clears to restore the American economy,” Brumage said. “But shame on us if we don’t invest in our public health infrastructure, and if we don’t invest in our overall health infrastructure, and if we don’t look for ways to make health care equitable for all Americans.”

