News
Kids Are Missing Critical Windows for Lead Testing Due to Pandemic
By: Brie Zeltner | Kaiser Health News
Posted on:
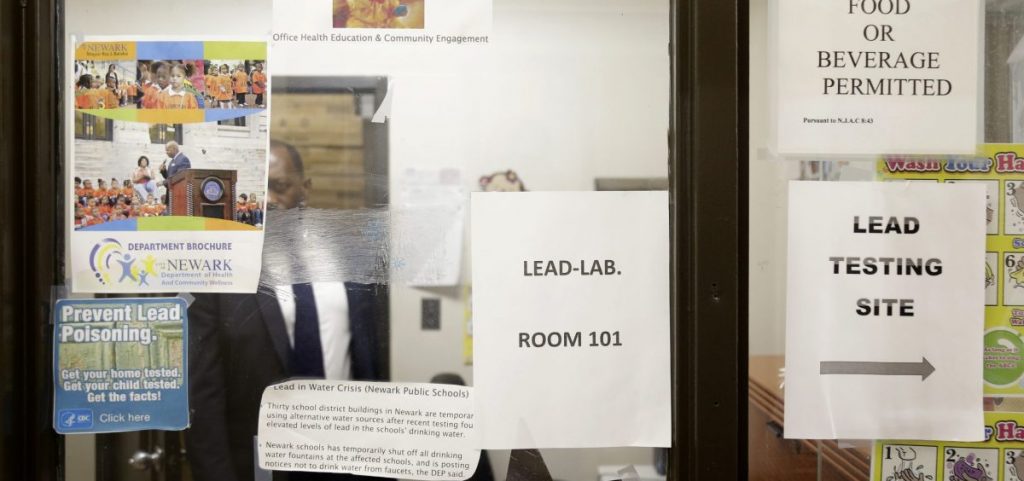
CLEVELAND, Ohio (Kaiser Health News) — Families skipping or delaying pediatric appointments for their young children because of the pandemic are missing out on more than vaccines. Critical testing for lead poisoning has plummeted in many parts of the country.
In the Upper Midwest, Northeast and parts of the West Coast — areas with historically high rates of lead poisoning — the slide has been the most dramatic, according to the Centers for Disease Control and Prevention. In states such as Michigan, Ohio and Minnesota, testing for the brain-damaging heavy metal fell by 50% or more this spring compared with 2019, health officials report.
“The drop-off in April was massive,” said Thomas Largo, section manager of environmental health surveillance at the Michigan Department of Health and Human Services, noting a 76% decrease in testing compared with the year before. “We weren’t quite prepared for that.”
Blood tests for lead, the only way to tell if a child has been exposed, are typically performed by pricking a finger or heel or tapping a vein at 1- and 2-year-old well-child visits. A blood test with elevated lead levels triggers the next critical steps in accessing early intervention for the behavioral, learning and health effects of lead poisoning and also identifying the source of the lead to prevent further harm.
“Inside is dangerous,” Hall said.
The CDC estimates about 500,000 U.S. children between ages 1 and 5 have been poisoned by lead, probably an underestimate due to the lack of widespread testing in many communities and states. In 2017, more than 40,000 children had elevated blood lead levels, defined as higher than 5 micrograms per deciliter of blood, in the 23 states that reported data.
While preliminary June and July data in some states indicates lead testing is picking up, it’s nowhere near as high as it would need to be to catch up on the kids who missed appointments in the spring at the height of lockdown orders, experts say. And that may mean some kids will never be tested.
“What I’m most worried about is that the kids who are not getting tested now are the most vulnerable — those are the kids I’m worried might not have a makeup visit,” said Stephanie Yendell, senior epidemiology supervisor in the health risk intervention unit at the Minnesota Department of Health.
Lifelong Consequences
There’s a critical window for conducting lead poisoning blood tests, timed to when children are crawling or toddling and tend to put their hands on floors, windowsills and door frames and possibly transfer tiny particles of lead-laden dust to their mouths.
Children at this age are more likely to be harmed because their rapidly growing brains and bodies absorb the element more readily. Lead poisoning can’t be reversed; children with lead poisoning are more likely to fall behind in school, end up in jail or suffer lifelong health problems such as kidney and heart disease.
That’s why lead tests are required at ages 1 and 2 for children receiving federal Medicaid benefits, the population most likely to be poisoned because of low-quality housing options. Tests are also recommended for all children living in high-risk ZIP codes with older housing stock and historically high levels of lead exposure.
Testing fell far short of recommendations in many parts of the country even before the pandemic, though, with one recent study estimating that in some states 80% of poisoned children are never identified. And when tests are required, there has been little enforcement of the rule.
Early in the pandemic, officials in New York’s Erie County bumped up the threshold for sending a public health worker into a family’s home to investigate the source of lead exposure from 5 micrograms per deciliter to 45 micrograms per deciliter (a blood lead level that usually requires hospitalization), said Dr. Gale Burstein, that county’s health commissioner. For all other cases during that period, officials inspected only the outside of the child’s home for potential hazards.
About 700 fewer children were tested for lead in Erie County in April than in the same month last year, a drop of about 35%.
Ohio, which has among the highest levels of lead poisoning in the country, recently expanded automatic eligibility for its Early Intervention program to any child with an elevated blood lead test, providing the opportunity for occupational, physical and speech therapy; learning supports for school; and developmental assessments. If kids with lead poisoning don’t get tested, though, they won’t be referred for help.
In early April, there were only three referrals for elevated lead levels in the state, which had been fielding nine times as many on average in the months before the pandemic, said Karen Mintzer, director of Bright Beginnings, which manages them for Ohio’s Department of Developmental Disabilities. “It basically was a complete stop,” she said. Since mid-June, referrals have recovered and are now above pre-pandemic levels.
“We should treat every child with lead poisoning as a medical emergency,” said John Belt, principal investigator for the Ohio Department of Health’s lead poisoning program. “Not identifying them is going to delay the available services, and in some cases lead to a cognitive deficit.”
Pandemic Compounds Worries
One of the big worries about the drop in lead testing is that it’s happening at a time when exposure to lead-laden paint chips, soil and dust in homes may be spiking because of stay-at-home orders during the pandemic.
Exposure to lead dust from deteriorating paint, particularly in high-friction areas such as doors and windows, is the most common cause of lead exposure for children in the U.S.
“I worry about kids in unsafe housing, more so during the pandemic, because they’re stuck there during the quarantine,” said Dr. Aparna Bole, a pediatrician at Cleveland’s University Hospitals Rainbow Babies & Children’s Hospital.
The pandemic may also compound exposure to lead, experts fear, as both landlords and homeowners try to tackle renovation projects without proper safety precautions while everyone is at home. Or the economic fallout of the crisis could mean some people can no longer afford to clean up known lead hazards at all.
“If you’ve lost your job, it’s going to make it difficult to get new windows, or even repaint,” said Yendell.
The CDC says it plans to help state and local health departments track down children who missed lead tests. Minnesota plans to identify pediatric clinics with particularly steep drops in lead testing to figure out why, said Yendell.
But, Yendell said, that will likely have to wait until the pandemic is over: “Right now I’m spending 10-20% of my time on lead, and the rest is COVID.”
The pandemic has stretched already thinly staffed local health departments to the brink, health officials say, and it may take years to know the full impact of the missed testing. For the kids who’ve been poisoned and had no intervention, the effects may not be obvious until they enter school and struggle to keep up.
Subscribe to KHN’s free Morning Briefing.

