News

Scientific Duo Gets Back To Basics To Make Childbirth Safer
By: Alison Kodjak | NPR
Posted on:
Brittney Crystal was just over 25 weeks pregnant when her water broke.
It was her second pregnancy — the first had been rough, and the baby came early.
To try to avoid a second premature birth, Dr. Joy-Sarah Vink, an obstetrician and co-director of the Preterm Birth Prevention Center at Columbia University Medical Center, arranged for Crystal to be transported by ambulance from her local Connecticut hospital to New York City, where Vink could direct her care.
Two weeks later Crystal started having contractions. She was given magnesium sulfate to stop them, and made it through the night. Crystal believed there was a future for her coming baby, whom she had named Iris.
“I went to the mirror and I talked to Iris,” Crystal says. “I said, ‘you know, this was a rough day. … You’re going to have them. But then the next day comes and the sun comes up and we move forward.’ ”
That evening, however, the contractions started again. Crystal was whisked to an operating room for a Cesarean section. She was a little under 28 weeks pregnant.
“I think I knew before I opened my eyes that she had died,” Crystal says, her voice cracking as she reaches for a tissue.
Afterward, as she was recovering in the hospital and mourning the loss of Iris, Crystal and her family asked a lot of questions. Why can’t you seal up the amniotic sac if your water breaks early? Why can’t you reliably stop preterm labor?
“And that’s when Dr. Vink told us that, you know, rare diseases are being cured in this day and age, but we don’t know what triggers full-term labor,” Crystal recalls. “That just collectively blew away everyone in the room.”
It was surprising but true. When it comes to pregnancy, research on some basic questions stalled decades ago, Vink says. If a pregnancy is normal, that doesn’t matter much. But when things go wrong, those gaps in knowledge become issues of life and death.
“It’s mind-boggling that in this day and age, we still don’t understand [even] in a normal pregnancy how women go into labor — what triggers labor,” Vink says. “Because we don’t understand the normal fundamental mechanisms, we can’t identify how things go bad — and then how we fix it when things go bad.”
Crystal, for example, had undergone a procedure called cervical cerclage: Vink had stitched Crystal’s cervix closed in hopes of preventing it from opening too soon. The technique has been around for more than 40 years, and it’s about the only treatment available for what doctors call “an incompetent cervix.” But much of the time, it’s not enough to stop a premature birth.
Most basic knowledge about pregnancy comes from research performed in the 1940s, Vink says, and she’s working hard to update that information.
She’s focused first on the cervix, she says, because if doctors can get the cervix to stay closed in those final, crucial weeks of gestation, the baby won’t be born too soon, even if the amniotic sac breaks.
“So, what is the cervix made out of? What proteins are there, what cells are there? How are all these things interacting? How do they change in pregnancy?” she asks, laying out some of the unknowns. By the end of pregnancy, a woman’s cervix goes from being stiff, like the tip of a nose, to very soft. But how?
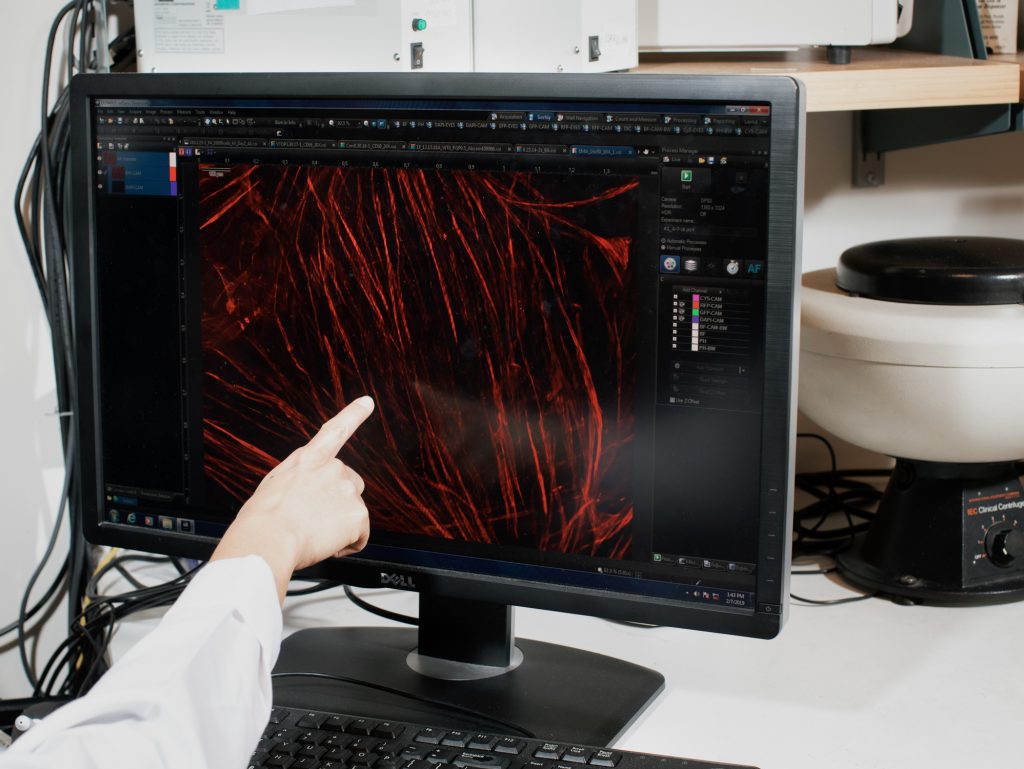
To help answer those questions, Vink and her graduate researchers are taking, for analysis, cervical tissue samples from women in her medical practice who are at different stages of pregnancy.
One of her first findings, she says, is that the cervix is not made mostly of collagen, as doctors long thought. It also has a lot of muscle.
While Vink studies what the cervix is made of, one of her university colleagues, mechanical engineer Kristin Myers, is trying to determine how it works.
“I’m kind of an oddball in the department of obstetrics and gynecology,” Myers says. “I teach mechanics classes and design classes here at Columbia.”
Myers got her start as an undergraduate, doing materials research in the automobile industry. Back then she tested how tires respond to heat.
That reaction reminded her adviser of how a bulging aneurysm bursts. He suggested she focus her curiosity on the mechanics of the human body. When she arrived at MIT for her graduate studies, Myers worked with researchers who were interested in the mechanics of pregnancy.
“It’s an important area — an understudied area — and a basic part of pregnancy physiology,” says Dr. Michael House, an OB-GYN at Tufts University who also has a background in engineering. “There is just lots to learn.”
House has been a mentor to Myers and continues to collaborate with her. He says the focus on the cervix is particularly important, “because a cervix problem can affect the pregnancy very early.”
About 1 in 10 babies are born prematurely in the U.S. each year. If those babies are born close to term — after around 35 weeks — they can do quite well. But a woman with a problematic cervix can go into labor much sooner, which can lead to miscarriage or a baby born so early that the child may die or face lifelong health problems.
Myers is investigating several aspects of the biomechanics of pregnancy — from how much the uterus can stretch, to how much pressure pregnancy exerts on the cervix, to how much force a baby’s kick puts on the whole system.
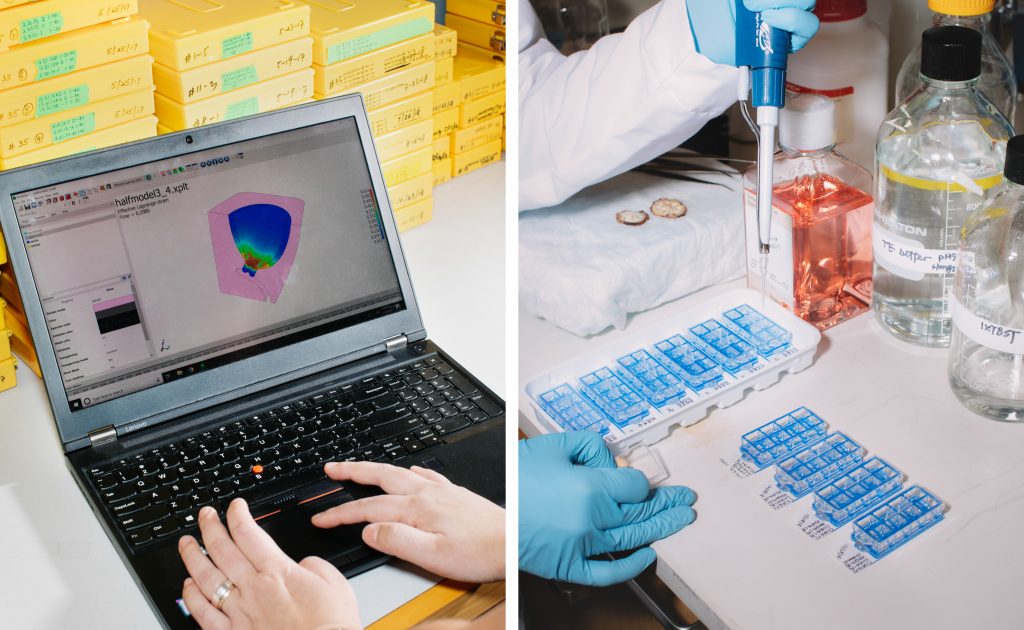
“We’re building computational models of female pregnancy to answer those questions,” Myers says.
She has two labs at Columbia — one at the hospital and one in the engineering school. In the lab at the engineering school there are a variety of microscopes and scalpels and slides. There’s one machine that can inflate the uterine membranes like a balloon, and another, about the size of a microwave, that stretches uterine tissue between two grips.
“These [are] types of machines you’ll see in all different kinds of material testing labs,” Myers explains. “In civil engineering you can have one of these machines that is like two or three stories high and they’re testing the mechanical strength of, [say], railroad ties.”
She is measuring just how much the cervical tissue changes during pregnancy — starting out with the capability and consistency of a tendon, and becoming something more like a loose rubber band.
“We’ve mechanically tested various pregnant tissues and non-pregnant tissues of the cervix,” Myers says, “and its stiffness changes by three orders of magnitude.”
Then the team uses their computer models to look at how the various factors — shape, stretch, pressure and tissue strength — interact as a woman moves toward labor and childbirth.
Their goal is to be able to examine a pregnant woman early on, and accurately predict whether she will go into labor too soon. It’s a first step, Vink hopes, toward better interventions to stop that labor.
That’s what Brittney Crystal is aiming for as well. After baby Iris died, Crystal started a foundation called The Iris Fund, which has raised more than $150,000 for Vink’s and Meyers’ research.
“She didn’t get to have a life,” Crystal says. “But we really want her to have a very strong legacy.”
9(MDI4ODU1ODA1MDE0ODA3MTMyMDY2MTJiNQ000))


