News
Why rapid COVID tests aren’t more accurate and how scientists hope to improve them
By: Maria Godoy | NPR
Posted on:
COLUMBUS, Ohio (Statehouse News Bureau) — How much should you trust the results of a rapid antigen test? That’s a question many people are asking these days amid recent research and anecdotes suggesting these tests may be less sensitive to omicron. Researchers are working fast to figure out what’s going on and how to improve the tests.
That includes people like Dr. Wilbur Lam, a professor of pediatrics and biomedical engineering at Emory University and one of the lead investigators assessing COVID-19 diagnostic tests for the federal government. His research team began evaluating rapid antigen tests against live samples of the omicron variant last December in the lab, and in early assessments, he says, some tests failed to detect the coronavirus “at a concentration that we would have expected them to catch it if it were another variant.”
That finding prompted the Food and Drug Administration to update its online guidance in late December to note that, while rapid antigen tests do detect the omicron variant, “they may have reduced sensitivity.”
A week later, a small preprint study found that in 30 people infected with the omicron variant, rapid antigen tests only detected a positive case two or three days after a PCR test caught it — and “sometimes even longer,” says Anne Wyllie, a microbiologist at Yale School of Public Health and one of the authors of that study.
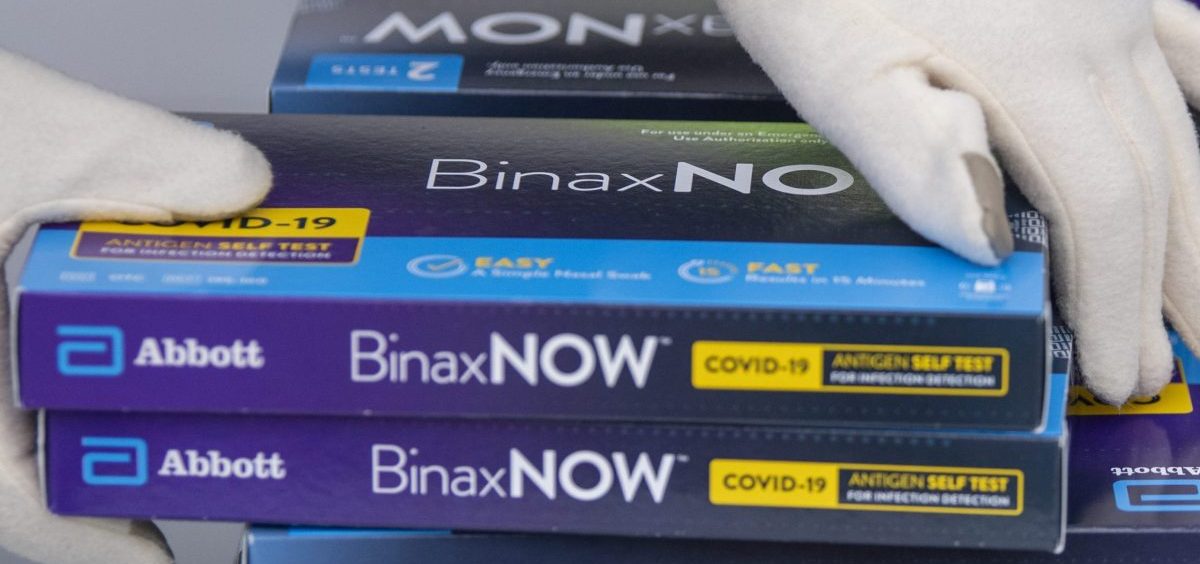
Rapid tests have always worked best when people are showing symptoms and have high viral loads, and so far, real-world data suggests they’re holding up well on that front. A recent study of 731 people found that the Abbott BinaxNOW rapid tests performed about as well with omicron as they did with other variants when people were symptomatic and had high viral loads.
Lam says that’s also what he’s finding when assessing rapid antigen tests with symptomatic patients who come into the clinic.
“These tests — they work,” Lam says. “When patients come in and they have symptoms …. we test them against the gold-standard PCR test and then we test with [a rapid test]. And by and large, with omicron, we see that they’re performing as expected.”
What’s different now is that with omicron, many people seem to be coming down with symptoms earlier on in an infection — before tests detect a positive case. Anecdotal reports abound of people showing symptoms of COVID-19 and testing negative at first, before eventually testing positive.

Such reports are puzzling, because you would think that if you’re sick enough to show symptoms, then the virus levels in your body would be high enough to register on a rapid test. But that’s not necessarily how it works. To understand what is going on, Lam’s lab is checking into several possibilities.
“This is all theoretical,” Lam stresses, but one idea is that people who are vaccinated start fighting off the infection as soon as it occurs. “And even though the virus may actually be living in the patient’s nose, the immune system might already be fighting it off, such that the viral load at that point in time of testing is too low to be detectable on the test,” he says.
Another possibility is that omicron might be showing up in different parts of the head first, so while at-home rapid tests require a nose swab, it could be that the virus is more heavily concentrated in your throat and mouth.
Lam’s lab is testing coronavirus-positive patients and their families daily with both PCR and rapid tests, taking samples from their throats, noses and mouths. The idea is to figure out when after an exposure people start showing symptoms, when their rapid tests turn positive — and which parts of the head have the most virus at different points in an infection.
“Hopefully, once we put it all together, we’ll be able to really answer the question of where does omicron live and when?” Lam says.
Another idea is that maybe some sub-variants of omicron produce fewer antigens — the proteins on the surface of the coronavirus that rapid tests detect — and that would make the tests less sensitive. To find out if omicron or some of its sub-variants produce less antigen, Lam’s team measures patients’ antigen levels.
Whenever patients test positive, the researchers genetically sequence their virus sample to figure out whether different omicron cases are genetically different. “If they are, could that actually be one of the reasons why some patients are detectable on rapid tests and some aren’t?” Lam says.
All of this information could potentially help rapid test manufacturers tweak their test design to make them more sensitive. For instance, if their data suggests that virus levels appear earlier or higher in the throat, Lam and his colleagues could recommend that the Food and Drug Administration ask test makers to add a throat swab to their test kits to make them more accurate. Lam says he thinks he will have enough data from patients within a few weeks to make a recommendation to the FDA.

“I think it would be incredibly shortsighted for companies not to work to expand their assays and also important for regulatory agencies to actually be pushing for this,” she says. In the U.K., rapid test kits already call for taking a sample first from the throat, then from the nose using the same swab.
She notes that a recent preprint study from the University of Maryland found that in the early days of an infection, virus levels were about three times higher in saliva samples than in nasal samples.
Down the road, rapid antigen test accuracy is likely to improve as researchers learn more about the kinds of variations that occur in the coronavirus proteins these tests target, says David Walt, an expert in medical diagnostics at Harvard University. That may allow test manufacturers to target areas of proteins that don’t vary, Walt told reporters at a recent briefing.
“Using computational predictions of protein variants, we’ll see some tests that are perhaps going to be able to be as sensitive across the board for all the kinds of variants that they encounter,” he says.
How to use the tests we have now for greatest accuracy
In the meantime, experts say there are ways to ensure we get the most accurate results possible from the rapid antigen tests we have today.
To start with, remember that these tests are most accurate when you’re symptomatic. That means if you have a limited supply of tests, and “if you have symptoms, assume that you are omicron-positive, and don’t use your one test that day,” Dr. Michael Mina, an epidemiologist and the chief science officer at digital testing company eMed, told NPR recently. “Wait a day, maybe two into symptoms to use your test because people are becoming symptomatic a day or so before they’re turning positive.”
Also, test serially. If you’re symptomatic but negative on the first test, wait a day — or two — then test again. If you haven’t been symptomatic for long, it may be better to wait two days, says Walt. He says there’s a good chance that by that time, “the virus will have replicated and your viral load will then be high enough to give you a positive result.”
If you’re negative after two rapid tests but still experiencing symptoms, consider testing a third time with a rapid test or getting a PCR test if you can, says Lam.
If you’re simply testing before gathering with family or friends, but you’ve got no symptoms or recent exposures that raise your probability of being infected, a single negative test is reassuring, but “it’s not just like an instantaneous free pass,” says Bruce Tromberg, who leads the National Institutes of Health’s RADx program, which aims to help the nation ramp up its testing capabilities.
Tromberg says a single negative test might make you feel better about running to the store with a mask on, or meeting a healthy friend for lunch. But if you’re using it to decide if it’s safe to visit your grandmother at the nursing home, don’t rely on a single test alone, he says.
“If I’m going to the nursing home on Saturday, I would start to isolate and reduce my social contacts in the preceding week, and I would take a couple of tests,” he says.
In other words, a rapid test provides helpful information in the moment. Just keep in mind that false negatives happen, so it makes sense to add other strategies to stay safe.
One final note: If you’re positive, consider yourself positive for real and isolate yourself. As a recent study found, false positives are quite rare.
Pien Huang contributed to this report.
9(MDU1ODUxOTA3MDE2MDQwNjY2NjEyM2Q3ZA000))

