News

Masking Questions: How Pandemic Health Measures Became Politicized
By: Liam Niemeyer | Ohio Valley ReSource
Posted on:
MURRAY, Ky. (OVR) — Health officials and researchers say the science is clear: face masks can help reduce the spread of the coronavirus. Yet in the Ohio Valley, not all elected officials are in agreement on whether to mandate measures such as the use of face masks in public places.
In April, Republican Ohio Gov. Mike DeWine initially announced the mandatory use of face masks in retail settings, only to walk back the mandate during the next day’s press conference to say it was only a recommendation. West Virginia Republican Gov. Jim Justice recently said that mandatory use of face masks would be impossible to enforce and would “divide us.” Kentucky Gov. Andy Beshear, a Democrat, ordered face mask use in public, but people who don’t wear one won’t be fined, though businesses that require masks can turn away customers who aren’t wearing one.
The renewed discussion about masks comes as the nation hit a new high for daily COVID-19 cases, driven by rapidly increasing infection rates in parts of the South and West, especially Florida, Arizona, and Texas forcing new shutdown orders.
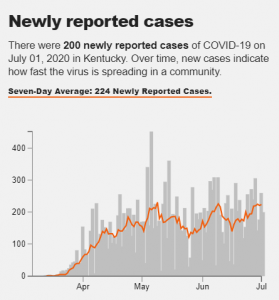
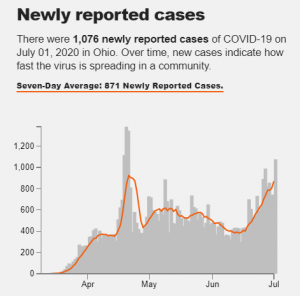
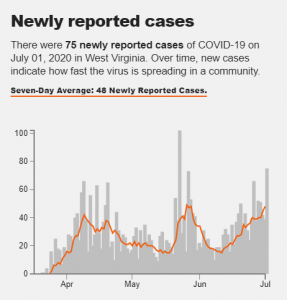
In the Ohio Valley, average cases per day have slowly risen over the last weeks of June, with daily totals now approaching levels last seen during the region’s earlier peak of the pandemic. Many rural outbreaks in the region have been linked to meatpacking plants, prisons, and nursing homes.
Besser addressed the politicization of public health measures, the high vulnerability to COVID-19 in the Ohio Valley, and what these factors mean for the future amid record high numbers of daily coronavirus cases in the country. This interview has been edited for brevity and clarity.
Liam Niemeyer: Should states mandate face mask use?
Richard Besser: This is a really challenging issue. I’m very concerned about mixed messaging. Every public health leader in America is out there saying it’s so critically important that we take all the steps we can to protect our health and the health of those around us. These are the early days in the pandemic, and what we do truly matters. So, that means wearing face masks when you’re outside and you’re going to be within six feet of other people. It means washing your hands frequently, staying home if you’re sick. But we are hearing mixed messages. I am hearing some Republican governors saying this as well. The Ohio Governor [Mike DeWine] was one of the early governors to shut things down in the state. I haven’t heard his messages about masks. But it’s very confusing to the public, and it’s very damaging to the nation when you see divisions along political lines around public health measures. When I ran Emergency Preparedness Response at the CDC, we did everything we could to try and not create a partisan divide around what we were recommending. And early on, you saw that here at the federal level with the C.A.R.E.S. Act, which was passed with almost unanimous support from both parties, providing supplemental unemployment insurance and eviction protection, and payment to small businesses, to keep them afloat.
LN: You mentioned the messaging regarding the Ohio governor. In April, Mike DeWine originally announced a face mask mandate for retail settings. But the next day during his press conference, he went back to say it would only be a recommendation. And West Virginia Governor Jim Justice has said recently he thinks face mask use will divide people.
RB: Yeah, from my perspective, there are real equity issues here. When you look at the impact of the pandemic so far, every community’s been hit, but some groups have been hit hardest: Black Americans, Latino Americans, Native Americans, lower income Americans, people in general who don’t have the choice about whether they’re going to work or not. And I think it’s our responsibility to do everything we can to protect people who must be in the workplace. So for me, if I’m going to the grocery store to get some groceries, I just think it’s a respectful thing to be wearing a mask so that the person who’s in that grocery store stocking the shelves next to me, who’s being exposed to hundreds of people every day, that I’m doing everything possible to protect that person’s health. If we can unify around that and say it’s the ‘American way’ to be, this idea of looking out for each other, it strikes me that there’s a core value there that spans across humanity.
LN: Moving to a related topic: a Kaiser Family Foundation study from April estimated how vulnerable populations in each state were to severe illness from COVID-19 due to pre-existing health conditions. The Ohio Valley had the highest rates of vulnerability in the country, with about half of all West Virginians at risk for severe illness. How does that vulnerability relate to still rising case numbers right now in rural America?
RB: It’s hard to paint rural America with broad brushstrokes because of the incredible diversity and richness of cultures, but there’s some things that you can say: there are higher rates of people who live in multi generational households. So, if one person is out working as an essential worker, and gets the illness and they’re young and they’re healthy, they’re going to be fine. But they may bring it home to somebody else who is elderly, or or somebody who has heart disease, lung disease or diabetes. There are very high rates of diabetes in Appalachia. So, from a medical side, there’s high risk. There are real challenges in terms of access to health care, as we’ve seen a lot of rural health facilities closing around the country. You see a high proportion of low income workers who don’t have the opportunity to work remotely from home…so these factors all combine to increase the risks in many parts of rural America, and the solutions for those problems may be different. We put together five principles for equitable restart of the economy for state, local officials. One of those is the importance of working with communities and understanding communities and what the needs are.
LN: There was another recent report by NPR that showed Kentucky and Ohio didn’t have enough contact tracers needed for their populations. What are the implications of this?
RB: Contact tracing is a critical piece as we move from lock down to opening up because when you switch and say ‘okay, we’re no longer gonna be operating on this idea that everyone stays home except essential workers.’ What you have to have happen is what’s happened, you know, the approach that’s used in many other countries where you identify cases quickly. So, testing available in every community and you’re doing, you’re looking at the numbers to make sure no communities are being left out on that testing. And then once you find someone who’s infected, you can very quickly identify who all the people they’ve had contact with close contact with. So those people can be aware and they can be provided with services. So they can be under quarantine, in case they get sick. You know, it’s a simple model, but each one of those pieces requires resources. And, you know, we’ve yet to see any of the states that have really seen their numbers come all the way down, make the transition over to this yet…and it’s not just having the number of contact tracers. That’s really important. But you want those contact tracers to be from the communities in which they’re operating, so there’s a level of trust. What we’re seeing in some places is that people don’t want to tell the contact tracers who their contacts were.
LN: What general advantages do regions like the Ohio Valley and Appalachia have in regards to this pandemic — isolation and sparse populations — and is that necessarily enough to dissuade more outbreaks in this region going forward?
LN: We have a couple of questions submitted by listeners to the Ohio Valley Resource through its member stations. This one was submitted by Paula Gill to West Virginia Public Broadcasting: how often do you need to change a mask if it’s only worn once every two weeks for an hour? So, how often do you need to sanitize a mask?
RB: When I looked at the recommendations on that from CDC and others, their recommendation is if it’s a cloth mask, It’s a good idea to have more than one and to throw it in the laundry and and wash it after each time of use. And you’ll be able to see online recommended ways of taking off and putting on a mask so you’re taking off a mask and you if you throw it in the laundry with your wash. That’s a good time to wash your hands because you’ve touched this mask that may now be contaminated.

RB: Not very. Those activities that you’re doing are very safe. You know, the nice thing about being outdoors, you know, if you’re outdoors and six feet away from people, it’s a really safe way to be, and it feels good. So I think your risk is very low.
Besser said individual decisions like wearing a mask can dramatically impact how many people will become sick or how many vulnerable people could die. He said wearing a face mask is ultimately about protecting one another, a small step that can make a big difference.


