News

The Real Cost Of The Opioid Epidemic: An Estimated $179 Billion In Just 1 Year
By: Selena Simmons-Duffin | NPR
Posted on:
There’s a reckoning underway in the courts about the damage wrought by the opioid crisis and who should pay for it.
Thousands of cities and counties are suing drugmakers and distributors in federal court. One tentative dollar amount floated earlier this week to settle with four of the companies: $48 billion. It sounds like a lot of money, but it doesn’t come close to accounting for the full cost of the epidemic, according to recent estimates — let alone what it might cost to fix it.
Of course, there’s a profound human toll that dollars and cents can’t capture. Almost 400,000 people have died since 1999 from overdoses related to prescription or illicit opioids. There are more deaths every single year than from traffic accidents. These are lives thrown into chaos, families torn apart — you can’t put a dollar figure on those things.
But the economic impact is important to understand. The most recent estimate of those costs comes from the Society of Actuaries and actuarial consulting firm Milliman in a report published this month.
“We pride ourselves that this is objective, nonpartisan research,” says Dale Hall, managing director of research at the Society of Actuaries. He adds, “we’re not here to influence any court proceedings.” As actuaries, they calculate financial numbers associated with risks, for instance, for insurance companies.
So how much did the epidemic cost in just one year, 2018? The total number they came to was $179 billion. And those are costs borne by all of society — both by governments providing taxpayer-funded services (estimated to be about a third of the cost) and also individuals, families, employers, private insurers and more.
Don’t see the graphic above? Click here.
When you start to break that number apart, a picture emerges of how opioid addiction ripples out into communities and across generations.
Overdose deaths: $72.6 billion
It makes sense that the biggest contributor to the costs of the epidemic comes from overdose deaths, according to Stoddard Davenport of Milliman, one of the report’s authors.
“When you think about the course of a person’s life that struggles with opioid use disorder, early mortality is the most significant adverse event that can happen, and I think that bears out when you look at the economic impact,” he says.
Every day, 130 people die from opioid overdoses. Most of them are in the 25-55 age range, right in the middle of their prime working years, and lost earning potential accounts for most of those costs.
“The mortality costs have a small component of end of life health care, coroner expenses and things like that,” he says. “The grand majority of it, however, is composed of lost lifetime earnings.”
Preliminary data suggest overdose deaths dipped in 2018 for the first time in years, but many experts say it’s too early to say whether that marks a turnaround.
Hall points out that whether the annual death toll stays as high as 47,000 in coming years “will be certainly a driver of what these overall economic costs will be.”
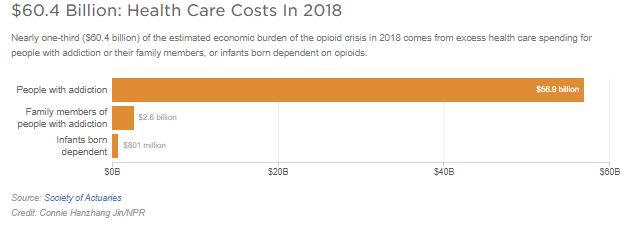
Health care: $60.4 billion
The next biggest amount comes from health care costs. The researchers took several large databases of insurance claims that had been scrambled to hide the identity of the patients and flagged people who had been coded as having opioid use disorder. Then the researchers calculated their overall health care costs — not just directly related to their addiction, but any additional costs — and compared them to similar patients without addiction.
Don’t see the graphic above? Click here.
“Looking at the difference in costs gives us a sense for how much more complicated is their overall health care picture and what those additional expenses look like for two otherwise comparable people,” Davenport explains.
Opioid addiction is linked to other health problems. Patients might have chronic pain or mental illness that underlies their addiction; infectious diseases like HIV and hepatitis C can spread among injection drug users; and there can also be higher costs for other conditions like anemia, liver disease and pulmonary heart disease, according to another Milliman analysis from earlier this year.

Then there are the costs for infants born dependent on opioids — what’s called neonatal abstinence syndrome. “The epidemic effect is starting to create a second generation that extends down to children and unfortunately newborns as well,” Hall says. In 2018 those costs were $800 million, but they estimate this year they could be almost $1 billion.
There are still more costs the report could not capture, including elevated costs for patients whose opioid use disorder is undiagnosed and potential ongoing expenses for children born with neonatal abstinence syndrome as they grow up.
Lost productivity: $26.5 billion
When someone is addicted to opioids, they might not be able to apply for or hold down a job, or they might be incarcerated and unable to work. The researchers broke this section out into reduced labor force participation, absenteeism, incarceration, short and long term disability, and workers’ compensation.
“What we’re trying to capture is the amount of time that folks are spending not doing economically productive activities,” Davenport says. Other productivity costs — like “presenteeism,” when someone shows up at work but isn’t as productive as they otherwise would be — were not included here.
It’s also worth noting, many of these costs fall to private employers, for instance, and families who have a family member not bringing home income.
“It’s around 30% falling on federal state and local governments,” he says. “The rest [falls to] the private sector and then of course to individuals.”
Criminal justice: $10.9 billion
Measuring this part of the costs of the epidemic is a different beast. The researchers captured costs related to police, court cases, correctional facilities and property lost to crime, Davenport explains. They drilled down into criminal justice expenses to see “what proportion of those total budgets involve substance use disorders, and then what proportion of that is represented by opioids.”
Having an opioid addiction dramatically increases the chance of being caught up in the criminal justice system. As NPR has reported, only 3% of the general population reported being recently arrested, on parole or on probation. For people with opioid use disorder, that jumped up to nearly 20%.
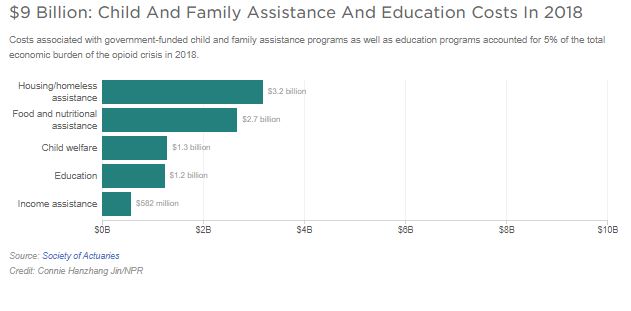
Child and family assistance and education: $9 billion
The team took a similar approach to calculate the costs for things like food assistance, child welfare, income and housing assistance, and education. They took those total costs, figured out what portion was related to substance use, and what part of that was related to opioid use.
The epidemic has a profound impact on families and communities — parents with opioid use disorder have to navigate treatment and sometimes battle for custody of their kids; the state has to handle child welfare cases and find new homes for foster kids; and schools are providing counseling for kids with addicted parents.
Don’t see the graphic above? Click here.
“Typically an epidemic will start in one place but then it broadens out,” says Hall. “We’re starting to see a broadening out of the impact of the opioid epidemic into some second generation effects.”
Hall adds there are also “the costs of educating people about the epidemic and ways to prevent future opioid use disorder.” Those costs — mostly from federal grants for elementary and secondary education programs — came out to $1.2 billion last year.
What’s missing: Turning the crisis around
These are some solid numbers that capture the current economic burden of the epidemic. Estimating what it’s going to cost to fix the crisis — to treat those who are addicted, to reduce overdose deaths, and more — is another story.
“The notion of abatement is that we want to deal with the problem that exists but also to begin to remedy it,” says Christopher Ruhm, professor of public policy and economics at the University of Virginia. He worked for several years on a 30-year abatement plan for Oklahoma as part of that state’s case against several drug companies.
For Oklahoma, Ruhm estimated treatment, prevention, education and surveillance for one year would cost $836 million. The judge in the case made his own calculations and ordered Johnson & Johnson to pay $572 million, though the amount has since been adjusted, and the case is currently being appealed.
If you scale Ruhm’s numbers up from that one state to the whole country, you get $69 billion to fund a year’s worth of abatement programs.
“I’m not saying that’s an appropriate calculation in the sense that things could be different in Oklahoma from other places,” Ruhm cautions. There are also costs that might come up on the federal level that wouldn’t be factored in for Oklahoma, such as research into effective addiction treatments.
Still, it gives you a rough idea, as society starts to take stock of what this epidemic is costing already, how much it will cost to try to fix it and who should ultimately pay.
9(MDI4ODU1ODA1MDE0ODA3MTMyMDY2MTJiNQ000))