News
Black lung patients and advocates urge mine safety officials to update silica dust standards
By: Katie Myers | Ohio Valley ReSource
Posted on:
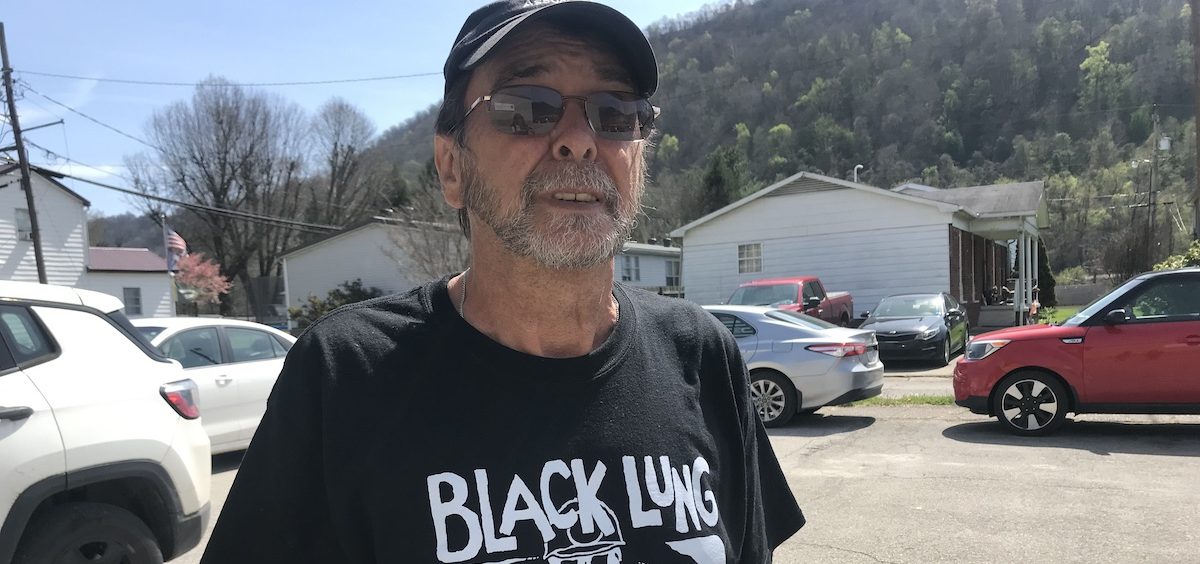
CABIN CREEK, W.Va. (OVR) — Jerry Coleman mined West Virginia coal underground for 37 years. When he was in his early fifties, he found himself gradually struggling to keep up with other men his age, and went to get checked out.
“Most people who look at you may think that you’re healthy,” Coleman said. “When you start getting black lung, you will notice that you can’t keep up with people. Your body just won’t let you do it.”
At 69 years old, Coleman has spent almost two decades living with black lung, struggling to breathe and straining against the close-fisted bureaucracies of the government and industry that promised to look after workers with the dreaded pulmonary disease.
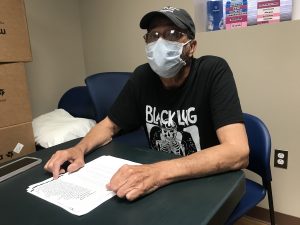
Sitting in a health clinic in Cabin Creek, West Virginia, Coleman wears a shirt with the national Black Lung Association’s signature logo — a skull in a miner’s helmet with the words “Black Lung Kills” splashed across the top. Breathing deeply before each sentence, Coleman recounted the lengths the company took to avoid paying his benefits.
“The companies will spend every dime they have to go to their doctors,” Coleman said. “Their doctors will do everything they can to say that you don’t have it.”
He spent nine years in the courts, battling the coal company that once cut his paycheck for a black lung diagnosis that would allow him to collect benefits and access treatment. He says that’s pretty average. Sometimes it takes longer. Sometimes miners give up trying. Some take years to see the doctor in the first place, dreading the truth, and dreading the years of litigation, testing, and doctor appointments that come with it.
According to a 2018 study in the American Journal of Public Health and the National Institute for Occupational Safety and Health, one out of five coal miners will develop black lung, which has no cure. One in twenty will develop progressive massive fibrosis, the most severe form of the disease, which is linked to silica rock dust. Over the years, the numbers have steadily increased. Now, new research shows the mine safety standards around silica dust have a lot to do with it.
A raging epidemic of black lung emerges
Coal mining has changed a lot since Coleman started in the 1970s. The ratio of rock-to-coal is different now, with miners encountering increasing amounts of rock, especially quartz, which is the source of silica dust. According to Coleman, the kind of coal that gets mined now was once viewed as “trash coal,” but now, it’s the standard.
“The coal mines now are mining coal that they never did want before,” Coleman said. “It’s lower. They’re taking more rock.”
Coal mining is more mechanized now, too, using a machine called a continuous miner, which grinds up coal and rock into the fine dust that can burrow deep into coal miners’ lungs. While these machines are not new, they have become more efficient at cutting rock over time, leading to increased dust in the mines.
Coleman says when he worked underground, safety inspectors visited on occasion, but companies tended to clean up their act when they knew an inspection was on its way. And miners faced retribution for expressing their concern.
“If an inspector is there, it’s different,” Coleman says. “Once he leaves, production is, is number one, you know, the men don’t have a lot of choice. If you backtalk them too much, next day… they’ll discharge you.”
In 2018, researchers uncovered the biggest cluster of black lung cases ever documented, located in central Appalachia. And those who diagnose the disease say the surge hasn’t stopped.
In the Pikeville United Medical Clinic in eastern Kentucky, radiologist Brandon Crum says he’s seen an increased number of black lung cases this year, compared to 60 in 2016, when he initially released research on increased black lung incidence.

During a recent interview, Crum recounted a case of a man in his thirties who needed a lung transplant, something he says would have been unthinkable a generation ago.
“I’ve seen more complicated [black lung] in the last 18 months than I’ve seen in my entire career reading black lung X-rays,” Crum said.
Even if coal mining stopped today, Crum says miners and their families will deal with the fallout for decades to come.
“All this complicated disease that we’re seeing in 30, 40, 50 and 60 year-olds, somebody’s going to have to take care of them for the next 20 or 30 years, and it’s going to be a huge burden,” Crum said.
Advocates hope new research leads to action
Coleman knew the fine silica dust he breathed every day had something to do with his condition, but he couldn’t prove it—until now.
Dr. Robert Cohen, a pulmonologist at the University of Illinois at Chicago, recently published a study that compared lung tissue from current miners to tissue from miners in decades past. What he discovered was an irrefutable link between increased silica levels and increased black lung, in younger and younger miners. Cohen says the link is definitive.
“We have a sort of epidemiologic evidence from where the center of the resurgent disease is located in central Appalachia, which is where we see these high silica dust levels,” Cohen said in a recent interview
“I think we have enough evidence to control this.”
An investigation by NPR and Frontline in 2018 found that federal regulators have known about the dangers of silica for at least thirty years, but have taken little action to curb exposure. For decades, despite repeated urging from the National Institute for Occupational Safety and Health, the Department of Labor did not act. After increased scrutiny, the Department of Labor’s Office of the Inspector General released a report affirming the danger of silica dust exposure. Now, Cohen’s research on the surging black lung epidemic is putting pressure on the federal Mine Safety and Health Administration to develop an updated silica standard.
Elsewhere in the federal government, officials have recognized the updated dangers of silica dust. The Occupational Safety and Health Administration brought its exposure limit down from 100 micrograms of silica dust to 50 micrograms in 2014. MSHA’s remains stuck at 100, despite the fact that silica dust exposure in a mining environment is no different from silica dust exposure in any other job.

But mine safety officials are reviewing the standard, and a rule change could be on the horizon.
In 2019, MSHA issued a request for information on respirable silica, asking for data to support a new standard, or information about technologies available to accurately monitor silica in coal mining operations. In 2020, the Department of Labor’s inspector general notified MSHA that it was not sufficiently protecting coal miners from silica exposure, and recommended immediate action. Former MSHA administrator David Zatezalo responded that the agency did not agree with the recommendations, but would review them.
MSHA officials didn’t respond to a request for comment on this story. The agency is expected to issue a new proposed standard, which could appear on the Labor Department’s spring rulemaking agenda in the coming weeks. Advocates support any moves the agency makes towards a new standard, but some worry it won’t go far enough.
Will a new silica standard be enough?
Advocates including regional black lung associations and the Appalachian Citizens Law Center petitioned MSHA in 2021 to change the silica standard, saying that in ten years of federal inaction, the black lung epidemic has only gotten worse.
Wes Addington, an attorney who runs the black lung legal clinic at ACLC, says even if a new standard were approved, it could fall short.
“Just because they develop a rule doesn’t mean it’s going to be sufficient enough to protect future generations of miners from the same fate,” Addington said.
Addington says the new standard could still fail to match OSHA’s, or it might not be paired with increased oversight and improved monitoring. And if the rule is going to work, MSHA needs to look for better ways to monitor silica all the time, not just during inspections, he said.
Addington points out that over the years, MSHA has successfully reduced mining accident deaths, proving that action is possible.
“The risk of immediate mining deaths in coal mines has vastly improved from where it was 100 years ago, or even 50 years ago,” Addington said. “But, the long term exposure to deadly dust has essentially been a failure, especially in the past quarter century.”
But Addington says any change in the standard is better than none.
Meanwhile, the trust fund that miners draw from for benefits is careening into debt — up to $2.8 million per week. The rate of the tax that supports the Black Lung Disability Trust Fund was recently slashed in half. A measure within the massive Build Back Better Act would have boosted the tax, but Democratic U.S. Sen. Joe Manchin of West Virginia, has effectively blocked it from passing.
Advocates fear that as the black lung epidemic expands, more of the burden will fall on miners and taxpayers, rather than on the coal companies that promised to take care of them.

“If there was proper ventilation in every mine, if there was appropriate personal dust monitors on every working miner…we could stop this,” Will said. “And we wouldn’t have to worry about benefits and medical services.”
Like many in central Appalachia, Jerry Coleman saw the mines as the best way to provide for his family. But now, he has trouble enjoying the life coal bought him. He can’t walk up his mountain anymore, or hunt. Sometimes, if he plays with his grandkids too long, he loses his breath and can’t get it back.
“If you want to make a good living, the coal mines was the place to work,” Coleman said. He took a deep breath. “Yeah, I made a good living. But I’m paying for it now.”
Roxy Todd contributed reporting to this story.
This story is part of the “America Amplified” initiative. America Amplified is a national public media collaboration focused on community engagement reporting.

