News
Addiction In The Pandemic: Staying In Treatment While Staying COVID Safe
By: Corinne Boyer | Ohio Valley ReSource
Posted on:
LEXINGTON, Ky. (OVR) — Since 2012, the 2nd Chance Center for Addiction Treatment has served people in Lexington, Kentucky. The office sits on a busy street on the city’s north side. Similar to the heavy traffic that passes by, clients seeking treatment for substance and opioid use disorders steadily stream in and out of the building.
But in 2020, the clinic had to limit that flow of patients as it changed its protocols to adhere to COVID-19 restrictions. Group therapy and individual counseling meetings stopped. In-person meetings moved to online video calls as telehealth appointments became an alternative.

“I’m employed, and I do have a stable background and family. But still, the isolation is extremely tough, and it does weigh on you,” he said. (The client asked to remain anonymous because of the stigma associated with addiction.)
In a December interview, Dr. Tuyen T. Tran, CEO of 2nd Chance, said he worried that the pandemic would worsen addiction, relapses and overdoses.
“With the pandemic, we’re going to probably see a surge in the number of cases of patients experiencing suicidal ideation, increased patients with addiction,” Tran said. “And for those who have been stable in treatment, the increased need for isolation will result in multiple relapses.”
A week later, drug overdose death data from the Centers for Disease Control and Prevention affirmed Tran’s prediction. June 2019 through June 2020 was the deadliest year for drug overdoses the country has ever seen.
The Ohio Valley, an early epicenter of the opioid crisis, saw overdose fatalities soar, and in parts of the region the rate of increase surpassed the national average. But while the pandemic is compounding the addiction crisis, it has also catalyzed additional state and federal responses to the epidemic. From local clinics and state agencies to newly appointed officials in the White House, people are looking for ways to tackle both new and existing barriers to treatment during the pandemic.
Overcoming Barriers
When the pandemic first emerged, many addiction treatment programs went to a virtual setting online. But, as with many aspects of work and education, that shift exposed common barriers people face as economic inequality and infrastructure gaps restricted access to telemedicine visits.
“We take it for granted, everyone has a cell phone, everyone has a laptop or a computer. But that’s not necessarily the case,” Tran said. “And so we experienced many difficulties with getting our patients seen with telehealth.”
The lack of broadband internet access in parts of the region also impeded access to treatment. Tran’s clinic provided Wi-Fi access so people could safely participate in group therapy sessions from their cars in the parking lot. For patients who didn’t have a phone or internet, 2nd chance established isolated space in the clinic with a computer for telehealth visits.
The pandemic’s economic impact also started to affect their clients, as unemployment escalated and people lost income. Some were struggling to pay for rent, food and other necessities. The clinic helped out with unemployment insurance claims, job searches, and even referred some patients to food banks, as well as signing some up for Medicaid as well as signing some up for Medicaid, which, among other things, allows clients to continue to pay for treatment.
In addition to the multifaceted stress caused by the pandemic, stigma still presents a significant barrier to treatment and the acknowledgement of substance and opioid use disorders as chronic diseases.

Tran said Lexington area hospitals have worked to combat that stigma and treat addiction patients the same as anyone being seen at a hospital.
For a few months during the pandemic, Tran said, the clinic couldn’t monitor patients, which helps hold those in treatment accountable.
“Since they weren’t being monitored, they began to use additional illicit drugs, and we’ve been detecting them when we started monitoring again,” he said.

“So all these things cause all kinds of problems in the illicit drug market because people may think they’re injecting methamphetamine when in fact it’s a cocktail of methamphetamine and fentanyl,” Ingram said. “They may think they’re taking a pharmaceutical drug when they’re not.”
Tran fears that the number of fentanyl analogs, or various chemical structures, will complicate drug screenings.
“To detect certain analogs, you have to have the proper reagents,” Tran said. “Well, the new analogs are coming out so rapidly, we can’t keep up with creating reagents to test for them.”
If fentanyl analogs evade drug tests, it can complicate treatment for patients possibly leading to more drug overdose fatalities, Tran said.
State, Federal Efforts
West Virginia has long had some of the nation’s worst rates of addiction and overdose deaths, and federal data show the death toll has surged during the pandemic.
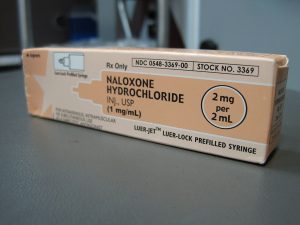
Last year West Virginia was awarded $43.7 million in State Opioid Response grant funding from the U.S. Department of Health and Human Services. So far, that’s assisted in the statewide distribution of approximately 28,000 doses of the overdose-reversal drug Naloxone.
“To be completely honest, our goal was to stop deaths so that we could get people into treatment or back into treatment,” Christina Mullins said. Mullins is Commissioner of the Bureau for Behavioral Health in West Virginia’s Department of Health and Human Resources, “We expect people to relapse. This is a chronic disease where relapse happens.”
“And since the pandemic started, we’ve run over 7,700 of those deviated routes, getting people back and forth to where they need to be,” Mullins said. “That has been one of the biggest challenges in my public health career.”
At the federal level, health officials just beginning their duties in the Biden administration know that more people with substance use disorder need access to treatment. Regina LaBelle is the acting director of the White House Office of National Drug Control Policy, which develops and oversees the administration’s National Drug Control Strategy and budget.
“We have to develop a treatment infrastructure around this country that makes sure that we can get people the treatment they need, the services they need, when they need it,” she said. “And we’re just not there yet. I mean, there are 20 million people in this country who have some form of substance use disorder, and only about 11% of people get treatment.”
LaBelle says the pandemic has allowed for some policy revisions that have improved access to treatment, such as telehealth.
“The ability to do Telehealth has been kind of a game changer for their ability to connect with their patients. And it’s really helped to retain people in treatment during this very uncertain time.”

“That we recognize that how we treat someone, a person of color, in one part of the country may not be the same as that type of treatment or other services the person needs in another part of the country,” LaBelle said.
She added that expanding that treatment is part of “the whole government approach to racial equity that the Biden-Harris administration is taking on.”
LaBelle echoed the importance of some of the work already underway in the Ohio Valley, such as expanding the availability of Naloxone and providing transportation assistance for rural patients.
She said her office will be reviewing some of the temporary policy changes that have been made to address needs during the pandemic with an eye toward which of those changes should be made permanent.
In Treatment
The experience of clients at Lexington’s 2nd Chance clinic drive home just how urgent those efforts will be as the pandemic wears on.
The anonymous client who spoke with the ReSource said extended isolation is a challenge for him as he manages his opioid use disorder, and he said it can affect addiction of any kind.
“You’ll probably see a large increase in people with addiction and needing recovery,” he said. “Anytime you have people with addiction, and they’re being forced to stay at home or out of [work], I think it’s going to create a bit of a problem.”
He hasn’t attended recovery meetings like he once did because he helps elderly members of his family. The pandemic has forced him to further limit his contact with others so as to reduce the risk of transmitting the virus to highly vulnerable people.
“By visiting, helping them with groceries, I’m over there taking them to the doctor when they need help,” he said. “Things like that have really kept me from attending meetings, like I would have in the past prior to the pandemic, just because of the fear of me being asymptomatic and transferring the disease to someone and someone I really care about passing away because of me.”
He has stayed in touch with his recovery group and sponsors by using social media, but he doesn’t think the public has “broad knowledge of what people with addiction go through, what the disease is. So I think, definitely, people with addiction are kind of left behind in so many ways.”
This is the second story in a series of reports about the addiction crisis during the pandemic. Part three will examine solutions regional experts are developing to expand treatment and reduce overdose deaths.
The Ohio Valley ReSource gets support from the Corporation for Public Broadcasting and our partner stations.


