News
COVID testing FAQ: When to test, what kind of test to use and what your results mean
By: Melody Schreiber | NPR
Posted on:
Each week, NPR answers frequently asked questions about life during the coronavirus crisis. If you have a question you’d like us to consider for a future post, email us at goatsandsoda@npr.org with the subject line: “Weekly Coronavirus Questions.” See an archive of our FAQs here.
WASHINGTON, D.C. (NPR) — In an ideal world, the U.S. would be awash in COVID tests. Anyone exposed to COVID could self-test and/or go to a lab or clinic for a test if necessary.
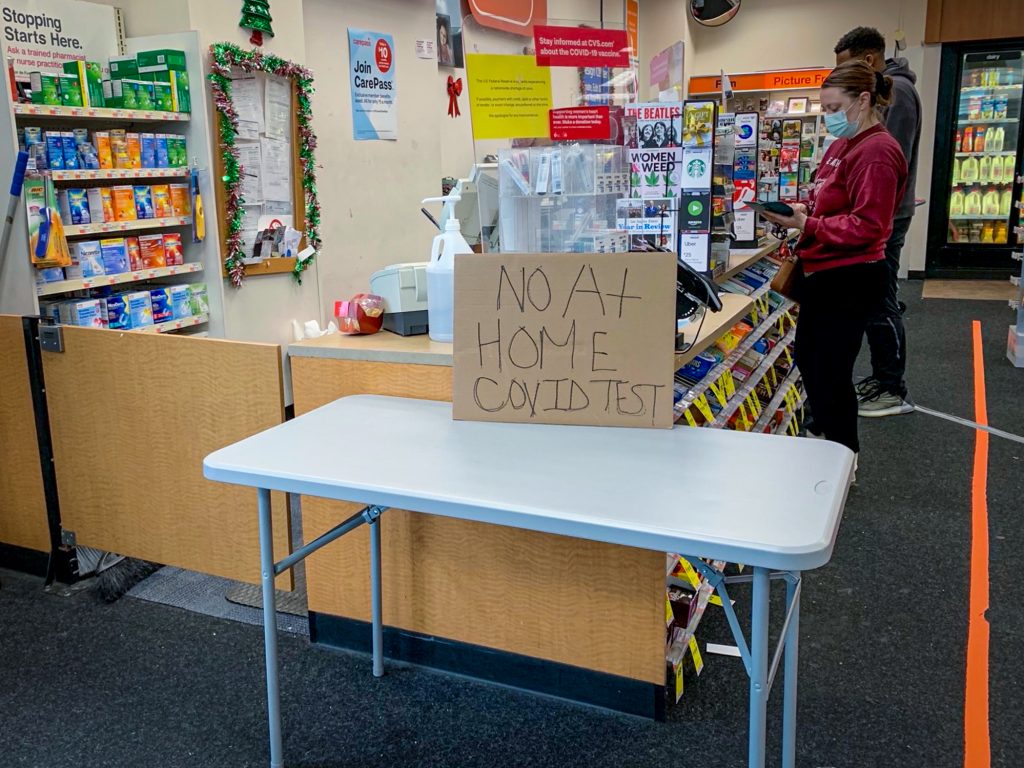
But right now, self-tests are in short supply in many parts of the country.
The Biden administration is pledging to distribute 500 million rapid tests “within weeks,” White House coronavirus response coordinator Jeff Zients said on Wednesday, but few other details have been announced.
And test manufacturers are ramping up production, so the hope is that at some point – although no one can say exactly when — you won’t be seeing those “no tests available” signs at the local pharmacy or have to wait a week or more for tests ordered online.
What’s more, the Centers for Disease Control and Prevention has changed its testing guidelines in the wake of the omicron surge in the U.S. — and public health researchers are critical of some of the recommendations.
The end result is a lot of confusion about testing — and a lot of frequently asked questions. Here are some answers to queries you might have about COVID tests.

What types of COVID tests are there?
There’s the rapid, do-it-yourself home test, which involves swabbing your nose and takes about 15 minutes to display a result on a test strip provided in the kit. These cost about $20 for a package of two tests. They’re known as antigen tests — antigens are basically the proteins from the virus that the rapid tests can identify.
Then there’s the PCR test performed in a lab or clinic. PCR stands for polymerase chain reaction, which is a technique for amplifying trace amount of virus DNA. Depending on how busy your local technicians are, you may have PCR results within a day or it may take several days. A PCR test usually costs about $150 without insurance.
Are there any other types of tests?
There’s a third type of test: a blood test that looks for antibodies after you’ve been sick, and some samples can even be taken from a finger prick at home and sent to a lab. But they are not used to diagnose COVID-19.
Does insurance cover testing?
Most insurance policies cover PCR and rapid tests administered by health providers. The Biden administration has announced a plan for insurance companies to reimburse at-home tests starting this month, but details are not yet available.
What’s the difference between antigen and PCR tests?
The PCR test is much more accurate at identifying an infection because it can amplify traces of the virus – in other words, even if you have a small amount of virus, it can detect it. So it can tell if you’re infected even a day or so after you develop what appear to be COVID symptoms or a few days after exposure to someone with COVID.
The antigen tests don’t magnify the amount of virus in the sample you take, so you need a pretty high viral load to test positive. As Susan Butler-Wu, associate professor of clinical pathology at the Keck School of Medicine of University of Southern California, puts it: “It’s a test for [determining if you have] a lot of virus.”
So you might test negative on a home test even if you are infected – for example, at the beginning or the end of your illness when you don’t have a lot of virus.
So which test should I go for?
The more urgent question, says Butler-Wu, is: “Which test can you get?”
If you have symptoms and likely been exposed to the virus by traveling or socializing, a positive antigen test is probably enough evidence that you have the virus, says Dr. Abraar Karan, an infectious disease physician at Stanford University.
As for PCR tests: Availability depends on the demand in your community. Some testing facilities are slammed, with few appointments available and hours-long waits even if you can snag an appointment. And it can take several days to get results from a PCR test.
What should I do while awaiting PCR test results?
While you’re waiting for test results, if you have symptoms, you should act as though the test is positive and quarantine.
If you’ve been exposed but don’t have symptoms, the CDC says you can go out while wearing a well-fitting, protective mask if you’re vaccinated and boosted.
Those who aren’t vaccinated should quarantine after a known exposure until test results are in.
(See this story for guidelines about quarantining or self-isolating after an exposure.)
When should I test — and how many times?
Of course, the answer depends on whether you can get tests – and what you’re using them for. Tests can be used to tell you if you have COVID – for instance, if you have symptoms or you’ve been around someone who tested positive. And they can also be used as an added precaution before socializing (which we’ll discuss a couple of questions down).
If you’ve been exposed to someone with COVID, you should self-test. But not right away.
“If you’ve been exposed, wait a few days because testing right away could be negative,” Karan says. After you wait, “then we’ll be able to detect virus.”
The Centers for Disease Control and Prevention recommends testing either when symptoms develop, or, if you aren’t showing symptoms, 5 to 7 days after exposure. That would give enough time for the body to develop a viral load that can be detected by a test.
With the omicron variant, there have been reports that rapid tests are negative during the first day or two of symptoms. So even if you’re showing symptoms, you might want to wait a day or two to take the first test, especially if you have a limited supply of tests.
How many tests should I take?
At least two.
Why test twice? Home tests are most accurate when you use them serially – at least two over the course of a few days. And if you have a limited supply of home tests, you will want to aim for the time when you are most likely to get an accurate result — say, on day 5 and day 7 after exposure.
“These tests absolutely have to be used serially, to be perfectly honest. They don’t have the sensitivity to be used one-and-done if they’re negative,” Butler-Wu says. “By repeating it, you’re allowing the virus to potentially grow more to the point, essentially, where now you can detect it.”
“If that test is negative, all that’s telling you is: At this point in time, you don’t have a ton of virus in you,” Karan says.
Should I get tested before seeing people?
“If you’re going to visit Grandma or something, yeah, I would probably rapid-test before that,” Karan says. “Or if I’m going somewhere where there’s going be a lot of people. If I’m contagious that day [and don’t know it], I could infect tons of people.”
A positive test result will tell you to cancel your plans and stay home and isolate.
But negative results don’t mean it’s time to rip the mask off in social settings. Rapid tests could be negative before a party and positive during it, just a few hours later – even if you’re vaccinated and boosted.
“To say that the negative test means being indoors unmasked – I think that needs to get rethought, pronto,” Butler-Wu says.
“Omicron has changed the game completely,” she says. “We know from Christmas soirees that occurred in European places that those exact scenarios happened: Vaccinated people, negative tests and there was still spread.”
If I test negative — how accurate are negative tests?
There can be false negatives, especially soon after exposure when not much virus is present in your body, or if the virus is replicating somewhere other than where you were swabbed – for instance, in your throat instead of your nose.
That’s why you should test at least twice.
According to a pre-omicron study, the Abbott BinaxNOW antigen test was 92.6% accurate at detecting the virus in symptomatic people and 78.6% accurate in asymptomatic people, compared to PCR results in cases where people had viable virus.
It is also possible to have a false negative from a PCR test.
“Any test is a snapshot of what’s happening in the part of your body that was sampled at that moment. That’s all it tells you,” Butler-Wu says. “So, yes, PCR is more sensitive in that it can detect lower amounts of the virus. But if you’re in the very early stages of incubating an infection and haven’t reached what we call the ‘limit of detection,’ that too, can be negative.”
What happens if I test positive?
When you test positive, you should isolate yourself for a minimum of five days and wear a mask for five days after that, according to the CDC. If you have rapid tests, you can use them after five days to see if you’re still positive, which would mean you need to continue isolating.
If you were tested at a clinic, they report the results to the local public health department for you. If you test positive on a home test, you should notify the health department so they can keep track of how many cases your community has.
Are there ever false positives?
False positives are rare on PCR tests and usually happen because of contaminated samples, research has found.
A false positive on an antigen test is possible but fairly unlikely if the test is taken correctly, says Butler-Wu – especially if you develop symptoms and you know you’ve been exposed to someone with COVID. And a lot of people are being exposed at this current time of great spread to the omicron and delta variants.
If “there’s a bunch of COVID and I’m symptomatic, it’s probably a true positive,” Butler-Wu says.
If you think you have a false positive from a home test, you can get a confirmatory PCR test – if you can find one.
“If your PCR is negative, then it’s possible that your rapid was a false positive,” Karan says. “If you’re able to do that, great.”
When else are PCR tests recommended?
If you are at risk for severe illness, you should get a test in case you need medication for COVID. And some workplaces and schools require a negative PCR test to return after travel or a non-COVID illness.
Do the tests detect omicron?
Rapid tests may not be as accurate for omicron, the U.S. Food and Drug Administration said in late December – but they haven’t released data yet on why they are less accurate and to what degree.
The FDA has also warned that three types of PCR tests may not detect omicron.
Because of these issues, if you’re testing at home after symptoms or an exposure to someone with COVID, the use of two tests spaced a few days apart is critical.
Can I use a rapid test to get out of isolation or quarantine early?
No. You should complete at least five days of isolation after you test positive.
According to the CDC, you may end isolation five days after testing positive, as long as your symptoms are “resolving,” including no fever for 24 hours, and you wear a mask “at all times when around others” for five more days.
The new guidance prompted criticism from public health experts. “I personally think a five-day lifting of isolation regardless of vaccination status, regardless of testing, regardless of anything – I am very concerned about it,” Butler-Wu says. “I’m just looking at how often people who have COVID still shed infectious virus at five days, and it’s quite a chunk.”
On Tuesday, the CDC changed those recommendations to include taking a test on day 5, if possible – but stopped short of requiring a test.
But if you do test at that point and test positive, continue isolating until you test negative.
“If you have COVID, and your antigen [test] is still positive at five days, you’re almost certainly still infectious,” Butler-Wu says.
And viral load isn’t the only factor for transmitting the virus – it also has to do with the situation you’re in and human behavior, like how much you are talking or singing and whether you’re masked, as well as environmental factors, like ventilation.
And what about taking a PCR test to end isolation?
PCR results can be positive for up to 12 weeks, because they don’t differentiate between viable and unviable viral particles – which means they may detect unviable virus after an infection has ended. So, a PCR test likely won’t tell you when to end isolation.
Melody Schreiber (@m_scribe) is a journalist and the editor of What We Didn’t Expect: Personal Stories About Premature Birth.
9(MDU1ODUxOTA3MDE2MDQwNjY2NjEyM2Q3ZA000))

